Health
Florence Kamette
-

Available versions :
EN
Florence Kamette
In France, where a national debate is ongoing [2], the over 65's represented 16.6% of the population and the over 80's 5.2% [3] in 2010. The "dependency ratio" [4], i.e. the number of people over 65 in relation to the number aged 15-64 lay at 25.81% in 2010. It is estimated at 39.02% in 2030 and 45.2% in 2060.
At present the dependent elderly are entitled to the "personalised autonomy allowance" (APA), which is paid by the "département" (county) and the monthly total of which depends on the recipient's degree of dependency, where they live (at home or in institution) and on their income. Hence for people living at home, the total amount varies from 530 to 1,235€ according to the degree of dependency. More than one million people over 60 receive the APA but the sums granted are generally inadequate particularly with regard to the recipients' ability to pay the fees of a specialised home. Therefore it is the families who still guarantee the major share of funding. Since the coverage of dependency by the social security – in the same way as other elements are covered (sick pay, pensions, family allowance and industrial injuries) – would lead to an increase in social contributions, the creation of a fifth social security category seems to be out of the question at present; it seems that the authorities are moving towards a dual solution which would call on solidarity for the poorest and on private insurance for the others.
The APA would therefore be reformed: the way it is attributed would be modified and the budget allocated increased by way of a second "journée de solidarité" (Day of solidarity with the elderly, established in 2004) or by an increase in the CSG (Contribution sociale généralisée, a tax that was established in 1990 and which helps towards the funding of the social security) towards retirement pensions. With regard to the optional subscription to a private insurance by people who are not eligible for the solidarity regime, incentives would be provided in the shape of tax rebates.
However nothing has been finally decided. Moreover the four working groups set up in January 2011 to look into how the loss of autonomy can be managed have to deliver their conclusions to the President of the Republic in July 2011 – the draft law on the funding of the social security for 2012 is due to be based on this.
This data justifies the present debate over the introduction of a fifth category within the social security regime – together with issues raised about the funding of dependency; this leads us to examine the measures with regard to the loss of autonomy by the elderly in several other EU Member States which have been selected because their social protection systems are inspired differently and offer more or less generous types of cover.
GERMANY
Demographic Data
In 2010, the over 65's represented 20.7% of the population and the over 80's, 5.1%. The dependency ratio represented 31.17% in 2010. It is estimated at 46.23% in 2030 and 59.08% in 2060.
The Public Dependency Care System
The 1994 Dependency Insurance Act, which came into force on January 1st 1995, covers all forms of autonomy loss, independent of the person's age. The dependency insurance system was reformed in July 2008 but without undergoing any radical change. Allocations were then re-weighted. In exchange social contributions, which are used to fund the measure, were increased.
Dependency insurance, the payment of which is obligatory, is incorporated into the health insurance regime: anyone who is affiliated to a statutory health insurance regime or to a private regime [5] is automatically affiliated to the dependency fund which is linked to his/her health insurance regime.
The 1994 Act qualifies three levels of dependency according to which benefits (physical care, home-help, etc.) are granted. The recipients of statutory dependency insurance can choose between benefits in kind given at home or in an institution, or cash benefits. However those insured with a private fund can only receive cash benefits. Benefits are granted independent of the person's income.
In addition to this, dependency insurance includes expenses incurred for specialised equipment (a medical bed for example) as well as expenditure - within a defined limit associated with housing.
Funding is guaranteed by social contributions that are shared equally between employees and employers and the rate of which is 1.95% [6]. In order to compensate for the employers' share a bank holiday was abolished in 1995 [7]. People who do not have children pay an additional sum of 0.25% and pensioners participate in the funding of the dependency insurance by way of a contribution that is equivalent to 1.95% of their pension.
The Number of Recipients
According to the Ministry of Health, in December 2009, 2.37 million people were receiving dependency insurance, 2.24 million of whom according to the statutory regime. Although the total amount of benefits in kind is greater than cash benefits (to avoid the misappropriation of funds) around 70% of recipients opt for the second type of benefit.
Since 1995 the number of recipients of statutory dependency insurance has increased in the following manner:
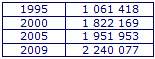
Around 70% of recipients of statutory dependency insurance live at home. Amongst these, one third receive benefits from private service providers whilst the others receive the aid of a relative who is remunerated in part thanks to the dependency insurance.
Outlook
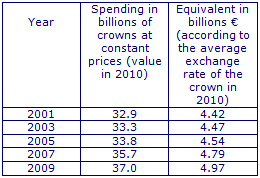
Expenditure on statutory dependency insurance in billions of € has increased as follows:
The financial results of the dependency insurance system, which were negative between 1999 and 2007 (except in 2006), lay at +0.99 billion € in 2009.
It is believed that there will be over 3 million dependent people in 2040. In October 2010, the Ministry of Health announced that a reform of dependency insurance would take place in 2011. It believes it necessary to supplement the present system, which is based on distribution, with a capitalisation system that will enable everyone to meet his/her own requirements in terms of their own degree of risk.
ENGLAND
Demographic Data
In 2009, the over 65's represented 16.3% of the population and the over 80's 4.6%. The dependency ratio lay at 24.72% in 2010. It is estimated at 33.23% in 2030 and at 42.14% in 2060.
The Public Dependency Care System
The 1990 National Health Service and Community Care Act establishes a clear distinction between care, which is the competence of the National Health Service, and assistance, which is the remit of the local authorities. To the latter it gives total competence for the entire care of elderly dependent people. Local authorities have to plan and organise the range of benefits on offer but are not obliged to provide them directly: they can turn to private service providers or fund the interested parties so that they purchase the benefits they need. As a general rule for people whose income rises above a certain threshold, the cost of these services are their entire responsibility [8]; in 2010-2011 the threshold lay at £23,250/year (i.e. around 27,000 € according to the exchange rate on January 1st 2011). Other recipients have to pay a contribution, the calculation of which varies from one place to another.
People aged at least 65 and who need assistance are entitled to an attendance allowance. The amount of this depends on the degree of dependency. Since 6th April 2010 it lies at £71.40 or £47.80 per week (i.e. around 84€ or 56€ according to the exchange rate on January 1st 2011). This allowance is granted independent of income and its use is not controlled: it is a supplement to income.
The Number of Recipients
In 2008-2009, 1.22 million people aged over 65 were receiving assistance in kind from local authorities; around one million were receiving assistance at home whilst the other were accommodated in specialised institutions.
At the end of February 2010, 58,523 people were receiving attendance allowance. There were 65,864 in 2001. Three quarters of recipients receive the maximum amount.
Outlook
The present system is not deemed very satisfactory; it is believed to be costly (£9 billion in 2008-2009 for local authority spending alone, i.e. around 10.5 billion € according to the exchange rate on January 1st 2011) and opaque. Indeed it is not clear that it serves the goals of independence and free choice of the elderly. The disparity in terms of the contributions paid to the local authorities is also criticised, likewise the fact that households have to pay a major part of dependency and that the system indirectly penalises savings.
The reform of the system has been planned for several years. The creation of a base for free care for all funded by taxes has been put forward by several working groups.
DENMARK
Demographic Data
In 2010, the over 65's represented 16.1% of the population and the over 80's 4.1 %. The dependency ratio lay at 24.98% in 2010. It is estimated at 37.85% in 2030 and at 42.66% in 2060.
The Public Dependency Care System
Managing dependency has not required the introduction of any specific measure. It is included in the social protection system: it is the result of an extension and progressive adaptation of the sanitary and social services according to the needs of the ageing population.
The Act on Social Services stipulates that everyone is entitled to free services he/she needs to maintain his/her quality of life, to remain at home as long as possible and to maintain both his/her physical and intellectual capabilities.
The municipalities [9] are responsible for the organisation of these benefits (home help, adaptation of the home or provision of adapted housing, day care in institutions, etc.) which are given free of charge and independent of the interested parties' financial situation. The local social services decide which types of benefits are necessary, but there is no formal tool to assess needs. Since 2002, recipients are free to choose the service provider which can be a private company.
Moreover, in order that the interested parties know what aid is available, the community must provide two annual visits to any person over 75 and who does not receive any type of assistance.
Since 1987, the Act on Social Services has prohibited the construction of any new retirement homes. [10]. On the other hand, adapted housing has been built. In addition to this, all new housing must be accessible to the handicapped and therefore to the elderly.
There are no cash benefits made to elderly dependent people, but an allowance can be paid to family members who help the elderly.
Since 1996, citizens over 60 elect a "senior council" in each municipality, which the town council has to consult before taking any decisions that may involve the elderly.
The funding of the entire dependency care system is guaranteed by local taxes and block grants from the State.
The Number of Recipients
In 2009, 182,265 over 65's (i.e. 20% of the over 65's) received aid at home. These benefits represented 668,108 hours/week, i.e. 3.7 hours weekly per recipient. Around 80% of the services provided came in the shape of personal care, and the elderly deplore that fact that they do not receive adequate aid in terms of domestic chores.
Around 4% of the over 65's live in a specialised institution. In this case, the interested parties pay a contribution equal to 10% or 20% of their income according to how important the latter is.
Outlook
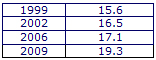
Spending devoted to the elderly has developed as follows over the last few years:
SPAIN
Demographic Data
In 2010, the over 65's represented 16.9% of the population and the over 80's 4.9%. The dependency ratio lay at 24.43% in 2010. It is estimated at 34.23% in 2030 and at 59.07% in 2060.
The Public Dependency Care System
The Act 39/2006, of December 14th 2006, on Promotion of Personal Autonomy and Care for Dependent Persons (LEPA) plans for the progressive introduction – since January 1st 2007 – of a dependency system that covers all forms of loss of autonomy, whatever the cause (age, illness, etc.).
The LEPA defines three types of dependency and divides each of these into two levels. It also defines the list of benefits in kind (from technical measures that aim to help people to stay at home to accommodation in a specialised institution) which must be offered to dependent people by the autonomous communities' social services and failingly that by private accredited service providers. According to the LEPA it is only if the direct provision of these benefits is impossible that financial allowances are paid.
The measure is based on the cooperation of the State and the autonomous communities [11]: the LEPA defines the framework in which the autonomous communities organise the care of dependent people and the State draws up conventions with the autonomous communities for the implementation of national measures.
From a financial point of view, the LEPA also plans for the cooperation of the State and the autonomous communities, since the autonomous communities' funds to finance the dependency measures must be at least equal to those of the State.
The State funds are split into two: on the one hand there is a contribution per dependent person and on the other an amount negotiated with each autonomous community. Moreover recipients participate in the funding of the measure according to their ability to contribute (income and property).
For every person who has been acknowledged as being dependent, the minimum State contribution, which is statutory, is as follows:
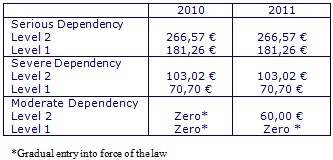
Moreover a decree determines yearly the maximum monthly rate of allowances that can be paid to dependent people. In 2011, these allowances were as follows:
As for contributions paid by the interested parties, these are determined by the autonomous communities as part of the rules established on a national level ; they depend on the nature of the benefit provided and so they vary enormously [12].
The Number of Recipients
On December 1st 2010, 654,499 people received at least one type of dependency allowance: 77% of them were at least 65 and 55% were over 80.
The allowance that is most frequently granted is aid to help pay a family member: some 380,000 people were recipients of this on 1st December 2010. Around 130,000 people received an allowance that was designed to cover accommodation fees in a specialised institution.
Outlook
In 2006, it was planned that national funds to finance dependency were to increase progressively from 400 to 2,212 million € over the period 2007 and 2015, with contributions on the part of the autonomous communities increasing in parallel.
In 2010, national funds for dependency totalled some 1,500 million €. They were deemed inadequate. The Observatory for Dependency published a study on 15th December 2010 in which it notably highlights the inadequacy of national funds which only cover one third of the entire system. The study insisted on the disparity in dependency care within the autonomous communities and on the exclusion of more than 200,000 people from the system.
ITALY
Demographic Data
In 2010, the over 65's represented 20.3% of the population and the over 80's 5.8%. The dependency ratio lay at 30.99% in 2010. It is estimated at 42.45% in 2030 and 59.32% in 2060.
The Public Dependency Care System
The public dependency system, which is secondary in comparison with informal aid provided by the family, is complicated and involves several types of actor: cash benefits are made by the State whilst benefits in kind are provided by the regions and municipalities.
Since 1988, the over 65's who experience "enduring difficulties" in undertaking basic daily tasks are entitled to an allowance that was previously reserved for the handicapped: they are entitled to receive support aid which is paid whatever the income of the interested party. In 2010 the monthly total of this was 480€. The use of this aid is not controlled: it comprises a supplement to income.
Benefits in kind are provided by the regions and the municipalities: sanitary services (accommodation in a specialised institution, day centres, etc.) are the responsibility of the former, the others are managed by both regions and municipalities (home equipment, home help, mobility aid, etc.). Some regions also provide cash benefits.
In 2007, public spending devoted to dependency was estimated at some 17.3 billion € i.e. 1.13% of the GDP. Support aid represents round half of this spending, accommodation in specialised institutions around 27% and home help 23%.
The Number of Recipients
It is estimated that 9.5% of the over 65's receive support aid, 3% live in specialised institutions12 and 4.9% receive home help12.
Outlook
Support aid has been criticised because it is a fixed sum: the amount does not take into account the degree of dependency.
As for benefits in kind, these vary from region to region and from one municipality to another. Generally aid structures and services to the elderly are much better provided for in the North than in the South.
The government believes that public spending devoted to dependency is too high and it is planning to promote subscription to private insurance companies. The National Dependency Fund, created by the finance law in 2007, which the State made available to the regions to enable them to guarantee a minimum level of aid, was abolished in 2011.
THE NETHERLANDS
Demographic Data
In 2010, the over 65's represented 15.3% of the population, the over 80's 3.9%. The dependency ratio lay at 22.82% in 2010. It is estimated at 40% in 2030 and at 47.18% in 2060.
The Public Dependency Care System
The system was reformed in 2007. Until the end of 2006 dependency care of the elderly was the responsibility of a sector of the health insurance system. It was covered under the Exceptional Medical Expenses Act (AWBZ: Algemene Wet Bijzondere Ziektekosten), which was a national obligatory insurance [13] initially designed to cover high risks that could not be insured. Not only did the system guarantee elderly dependent people long term care and accommodation in institutions, but also the provision of nursing services and home help. With regard to home care and aid since 1995 people can opt for a financial allowance instead of benefits in kind so that they can choose who their service provider would be. AWBZ spending is funded by social contributions. These have increased sharply over the last few years – particularly those related to social and household aid. This development is a result of the policy to keep the elderly at home [14] and from jurisprudence dating back to 2001 whereby people facing a loss of autonomy over a long period of time are entitled to request aid as part of the AWBZ.
The Social Support Act (Wet maatschappelijke ondersteuning : WMO), which entered into force on 1st January 2007, transferred responsibility for all non-medical assistance aid over to the communities [15] thereby reorienting the AWBZ towards the sanitary care of people that were severely handicapped.
The municipalities are obliged to set down a four year organisational plan with regard to their social aid work. In particular they have to compensate for the dependency of the elderly and handicapped by providing benefits designed to facilitate autonomy (notably equipping the home, delivery of meals, home help [16] and mobility aid) and by offering the interested parties the choice between benefits in kind or cash benefits. They have to set up a single point of contact which examines requests, defines the measures and if necessary establishes the level of cash allowances. Municipalities can ask recipients to participate financially – the sum of which the authorities are free to set, both in terms of its rate within the threshold set by law and the means of payment (lump sum or proportional to income, capped or not etc ...). Hence the share of someone over 65, living alone and whose annual income does not exceed 15,256 € is capped at 17.60 € for a period of four weeks.
The State pays the municipalities a grant calculated according the population's specific features. If they succeed in limiting social spending, the municipalities can use the funds available for other purposes.
The Number of Recipients
It is estimated that nearly 400,000 elderly people benefited from the AWBZ at the end of 2008. As for the number of recipients of home help as part of the WMO – although the figure is not final – it is believed that 55% of dependent people have either contacted the local WMO office or have received at least one benefit. The latest WMO assessment report, published in March 2010, indicates that the municipalities provided 600,000 new individual benefits in 2008, and that 250, 000 of these took the shape of home help.
Outlook
In 2010, the State grant for dependent people as part of the WMO lay at 1.3 billion €. In 2011, it is to be reduced by 200 million. The State justifies this reduction by the fact that in 2009 the municipalities only spent 86.6% of the grant which was allocated to them.
Recipients regret that some services in home are no longer provided by medical staff – which resulted after the entry into force of the WMO. Many services are now provided by home-helps or nursing auxiliaries and not by nurses.
With the exception of Spain, where the Act on Promotion of Personal Autonomy and Care for Dependent Persons has still not entered into force, the countries which guarantee the best care for dependent elderly people are Germany, Denmark and the Netherlands. However the State system in Italy is still secondary in comparison with family solidarity. As for the English system it is particularly complex and the organisation of services by the local authorities leads to major disparity in the benefits offered to the elderly.
[1] As part of devolution, Scotland and Wales established different systems so that several co-exist within the UK.
[2] http://www.dependance.gouv.fr/
[3] Except if the contrary is stated the demographic data quoted come from Eurostat.
[4] This strictly demographic indicator does not include either the real number of dependent elderly nor the increasingly late occurrence of dependency.
[5] Employees whose gross revenue is below a certain threshold (4,125€ per month in 2011) obligatorily depend on the statutory health insurance regime, whilst the others can take out insurance with another private regime, likewise independent workers and civil servants.
[6] 1 % in 1995 and 1.7 % between 1996 and July 2008. This rate applies to the gross capped salary, with the monthly threshold lying at 3,712,50€ in 2011.
[7] This was the Day of Penitence and Prayer, a variable bank holiday that was set around 20th November. This day is still celebrated in Saxony. In exchange the workers' share lies at 1.475% and the employers' share at 0.475%.
[8] Housing is included in the assessment of property except if the interested parties still live in the property itself.
[9] There are 98 municipalities, only 7 of them have under 20,000 inhabitants, 35 have a population ranging from 20,000 to 40,000 inhabitants, 50 have between 40,000 and 100,000 inhabitants and 6 have more than 100,000 inhabitants.
[10] There were only 9,436 places in retirement homes in 2009, whilst there were still 27,635 in 2001.
[11] In line with the Constitution, the State is competent to determine the conditions guaranteeing the Spanish equal rights.
[12] As an example the national law stipulates that people accommodated in an institution have to pay a maximum of 90% of their accommodation costs.
[13] The Dutch health insurance regime comprises two branches: national universal insurance, obligatory for high risk cases (long hospital sessions, chronic illnesses, etc.) and insurance for normal care. With regard to normal care the Dutch have had to take out insurance with a private insurance company since January 1st 2006.
[14] Between 1975 and1995, the percentage of people over 65 living in an institution declined from 9.6% to 6.9%.
[15] The municipalities, 418 in all, have an average population of around 40,000 inhabitants.
[16] Home help covered by the WMO only applies to household chores: help with personal hygiene is still covered under the AWBZ.
Publishing Director : Pascale Joannin
To go further
Gender equality
Fondation Robert Schuman
—
23 December 2025
Businesses in Europe
Olivier Perquel
—
16 December 2025
Digital and technologies
Josef Aschbacher
—
9 December 2025
Democracy and citizenship
Florent Menegaux
—
2 December 2025

The Letter
Schuman
European news of the week
Unique in its genre, with its 200,000 subscribers and its editions in 6 languages (French, English, German, Spanish, Polish and Ukrainian), it has brought to you, for 15 years, a summary of European news, more needed now than ever
Versions :






